Single-Day Design of Cases Detailed to an Active Pediatric Echocardiography Research Facility
Congenital and structural Interventionist, FCPS, FRCP (Edin), FACC, FSCAI, Combined Military hospital, Dhaka, Bangladesh
Correspondence to: Nahar Fatema, Congenital and structural Interventionist, FCPS, FRCP (Edin), FACC, FSCAI, Combined Military hospital, Dhaka, Bangladesh. E-mail: nahar_fatema4725@gmail.com
Received: April 02, 2023; Accepted: April 19, 2023; Published: April 25, 2023
Citation: Fatema N. Single-Day Design of Cases Detailed to an Active Pediatric Echocardiography Research Facility. Arch Med Res Health Sci. 2023;1(1):25-.
Copyright: © 2023 Fatema N. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ABSTRACT
Aim: In a busy pediatric cardiac outpatient and echocardiography unit, he identifies patterns of different types of heart disease in children reported daily.
Background: Congenital heart disease is a leading cause of childhood morbidity and mortality. This study was conducted to examine disease patterns in children referred from across the country to busy cardiac centers in Bangladesh. This is an observational study of his day in hospital. All patients underwent clinical examination and chest radiography. Electrocardiography was performed when indicated. The definitive diagnosis was made by echocardiography. All data were collected in the echocardiographic laboratory at the end of the day. While drafting this report, I noticed a certain pattern among the patients. On that day many patients came from different parts of the country and were representative of the population of the country, so the authors decided to publish this experience.
Methods: This was her one-day study of cases reported to a pediatric cardiac outpatient clinic in a tertiary care hospital in Bangladesh. This study included all patients with suspected or confirmed congenital heart disease.
Results: Of the 66 patients, 69.70% were male and 30.31% were female. 25 (41.66%) in the 1 month to 1 year age group, 21 (35%) in the 1 year and older age group, 13 (21.66%), and 7 (11.66) in the 5 and older age group. %) There has occurred) age group less than 1 month old. Atrial septal defect (ASD) was identified in 10 cases (15.16%), ventricular septal defect (VSD) in 9 cases (13.36%), and patent ductus arteriosus (PDA) in 8 cases (12.13%)., one fallow was confirmed. Tetralogy was observed in 3.03 of his cases. Down syndrome was present in 2 cases (3.03%) and congenital rubella syndrome and Crouzon syndrome in 1 case (1.51%). The most common surgery was PDA device closure (7.57%), with VSD closure and PDA ligation being the most common surgical procedures. Most cases (43.93%) remained on observation, 9 (13.63%) recommended surgery, and 8 (12.13%) recommended catheterization. Eight patients (12.13%) were discharged from follow-up due to spontaneous resolution.
Conclusion: The disease patterns observed in his one-day survey in a busy outpatient clinic showed patterns like those seen in other long-term studies. Most patients remained under observation because spontaneous healing could be achieved after observation in some cases.
Keywords
Pediatric Echocardiography, Pediatric Cardiologist, Pulmonary Artery Atresia, Syndrome.
INTRODUCTION
A congenital heart defect (CHD) is a structural malformation of the heart or large blood vessels present at birth. Regardless of the time of diagnosis, coronary heart disease is the most common malformation, accounting for approximately 30% of all malformations [1-5]. Congenital heart disease can occur alone or in combination with other disorders. Some flaws are simple, some are complex. A major congenital heart defect (MCHD) is a heart or great vessel defect that requires surgery or catheterization within the first six months of life. Pediatric cardiology was established as a subspecialty in Bangladesh in 1998, but initially, neither pediatricians nor the public knew that such a harmful disease existed in our community. did. All involved were then enlightened through ongoing medical training. A study conducted at the Integrated Military Hospital in Dhaka showed that the birth rate in our country was 25 out of 1,000 [4].
A study of infants in Baltimore, Washington found a birth rate of 4 in 1000 [5]. Cardiac fetal screening in early pregnancy and subsequent abortion of sick fetuses has contributed to the decline in incidence in Western countries. Maternal health and nutritional status are also better in developed countries. Although many hospital-based studies have been conducted in many parts of the world, there are limited studies in South Asia. Local experiences are emphasized in this study [1, 3, 5]. In this study, cross-sectional views of patients presenting to a busy pediatric cardiology outpatient clinic in Bangladesh during the day were taken for interviews.
METHODS AND MATERIALS
On the busy day of March 6, 2017, all patients presenting as referral cases to a pediatric cardiologist at a tertiary care hospital were randomly selected. All cases were examined by a pediatric cardiologist after a medical assistant measured the patient's weight and oxygen saturation. Each patient's cardiovascular system was thoroughly examined, and a preliminary diagnosis was made. Chest radiography and electrocardiogram (ECG) were recommended in some cases, but in all cases for anatomic diagnosis of new cases, follow-up of previous illness, or follow-up after procedures or surgeries. echocardiography was recommended. Patients were recorded in a database in a non-invasive laboratory. Adults presenting to a pediatric cardiologist with chest pain were excluded from participation.
Data was analyzed in Microsoft Excel. Numerical data were expressed as frequencies and categorical data as percentages. As this is an observational study with a single variant, no comparative analysis was required.
RESULTS AND DISCUSSION
Of the 66 cases, 46 (69.70%) were male, and 20 (30.31%) were female (Figures 1 and 2). Figure 2 shows the age distribution of the subjects. Seven (11.66%) were in the age group 0-01 months, 25 (41.66%) were in the 1 month to 1-year group, and 21 (35%) were in the 1-to-5-year group. Thirteen (21.66%) cases were in the age group ≥5 years. Figure 3 shows the general distribution of cases reported on that day. Fifty-eight (87.88%) had various types of congenital heart disease, 5 (7.57%) had normal hearts and 3 (4.51%) had simple CAD with spontaneous closure. I was. Figure 4 shows that 21% of patients are from large cities and 79% of patients are from peripheral and rural areas. Disease pattern in the cases studied. Ventricular septal defect (VSD) in 9 cases (13.63%), atrial septal defect (ASD) in 10 cases (15.16%), patent ductus arteriosus (PDA) in 8 cases (12.13%), foramen oval Presence (PFO). in 3 (4.56%) cases. One VSD and two ASD secondary cases resolved spontaneously. Among the complex forms of simple congenital heart disease, VSD with pulmonary artery stenosis (PS) was the most common (6.06%). Among cyanotic CAD mutations, tetralogy of Fallot (TOF) was the most common (3.03%), followed by transposition of the aorta (TGA) at 1.51%, pulmonary artery atresia (PA) at 1.51%, and dual exit right ventricle. (DORV) is 1.51%, trunk artery (TrA) is 1.51%, and so on. Among the neonatal special circumstances, persistent pulmonary hypertension was observed in 5 (7.57%) patients. No cases of fetal echo or adult congenital echo were reported on this day. The syndromic relevance in the case studies. Down syndrome was observed in 2 cases (3.03%), congenital rubella syndrome in 1 case (1.51%), and Curzon syndrome in 1 case (1.51%). The location of the heart in the analyzed cases. Left-sided heart disease was observed in 65 (98.48%) cases and right-sided heart disease in 1 case (1.51%).
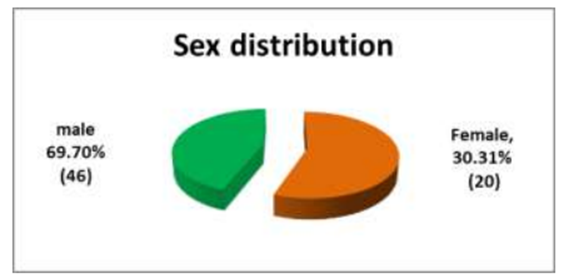
Figure 1: Sex distribution of patient.
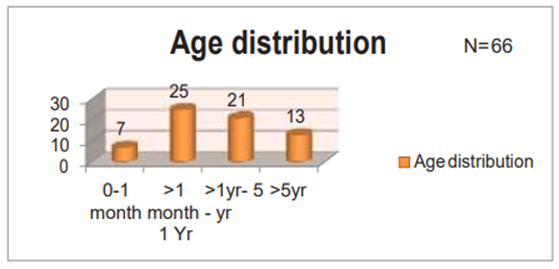
Figure 2: Age distribution of patients.
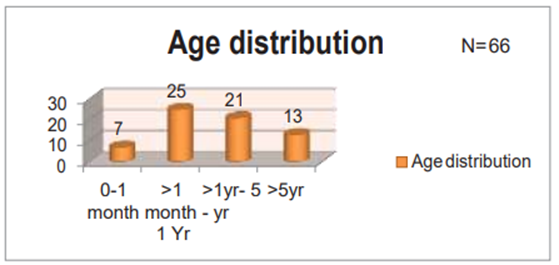
Figure 3: Distribution of patients.
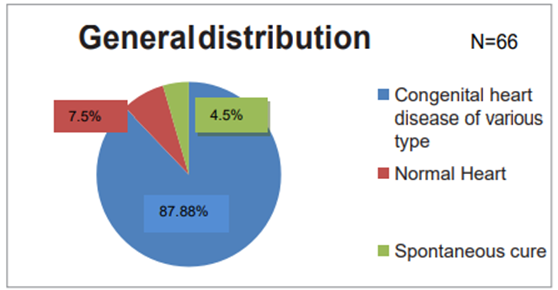
Figure 4: Distribution of patients based on locality.
The post-intervention follow-up cases in the study group. Five (7.57%) required epidural device occlusion, one (1.51%) required PDA stent placement, one (1.51%) required pulmonary balloon valvuloplasty, and three required 3-day post-protocol medical attention in persistent pulmonary hypertension (PPHN).) (4.56%) cases were identified. Surgical techniques in follow-up cases. VSD closure and PDA ligation were performed in 2 cases (3.03%), TOF repair, PDA ligation, septal myomectomy, bidirectional grain shunt (BDG) for mitral atresia, and DORV in 1 each It was done in the example (1.51%). The immediate treatment plan was provided after the patient's echocardiogram. Medical treatment was offered to 11 patients (16.67%), 29 (43.93%) were transferred to observation, transcatheter treatment was planned in 8 (12.13%), and surgical intervention was performed in 9 (13.63%). was planned. Case. Eight patients (12.13%) were discharged because of normal echocardiogram or spontaneous resolution of uncomplicated disease. One patient (1.51%) was found to be inoperable (AP window).
Congenital heart disease is the most common congenital malformation and causes the highest morbidity. A study of the incidence of congenital heart disease in hospital live births in Bangladesh found it to be 25 per 1000 live births [4]. Studies have shown that 3.9 out of every 1,000 births in India suffer from coronary artery disease [1,6-8]. In Pakistan, the incidence is 4/1000 live births [9]. A global analysis of incidence studies showed a consensus of 8–10 per 1000 live births. In our study, the predominantly male sex was determined (Figure 1). This was also observed in other studies [1-4, 10]. Most cases in this study fall in the 1-month-old to 1-year-old group (Figure. 2). In other studies, in most cases, the first saw a doctor in the first year of life. Studies by Nazma et al., Burki et al., and Khalil et al. showed similar results [2,11-12]. About the pattern of disease, the most common disease was ASD (15.16%), followed by VSD (13.63%) and PDA (12.13%). In Bangladesh, ASD was found as the commonest cyanotic lesion in other studies also13. Among cyanotic heart diseases, TOF (3.03%) was the most common even on that single day which correlates with other studies in India, Pakistan, and other countries [1-2,4,13,14].
The most common combination lesion in this 1-day data analysis showed that VSD and PS were the most common combination (6.06%). A similar pattern has been found in other studies [14]. Down syndrome was found to be the most common syndrome in this study, which is consistent with other studies. Medical and catheterization procedures were performed in 10 cases (15.16%), and surgical procedures were performed in 6 cases (9.06%). Other studies have also shown that the current scenario favors intervention over surgery [14]. The reason is that most procedures now give good results and parents always prefer non-surgical procedures for their children. The management plan (VI) was determined according to the patient's specific disease requirements. Most cases, mainly neonates and young children were included in follow-up because simple lesions had time to heal spontaneously. Treatment was offered to patients with heart failure, pulmonary hypertension, and associated chest infections. Cases with previously uncomplicated CHD cured were released from follow-up. Surgical intervention was offered in some severe and complicated cases and suggested in viable cases.
CONCLUSION
The experience of a single day in a busy tertiary care hospital echocardiography laboratory mirrors scenarios observed in different countries over the years. Various cases representing the entire country reveal how cases are managed in a country like Bangladesh. Complex neonatal procedures are referred to neighboring countries, but all types of medical procedures and catheterizations are performed at our facility.
REFERENCES
1. Rokeya Begum, Kumud Pathak, Himadri Das, Journal of Dental Medical Science2016; Vol15(06);8-11.
2. Najma Patel, Shama Jawed, Nagina Nigar, Fariha Junaid, Asia Abdul Wadood, Fatima Abdullah. Pak J Med Sci 2016; 32(1):79- 84.
3. Hoffman Julien IE, Kaplan The Incidence of Congenital Heart Disease. J Am Coll Cardiol. 2002; 39(12):1890–1900. Doi: 10. 1016/S0735-1097(02)01886-7.
4. Incidence of Congenital Heart Disease among Hospital live births in a Tertiary Hospital in Bangladesh. Nurun Nahar Fatema Begum, RB Chowdhury, Liza Chowdhury.CVJ2008;1(I):14-20.
5. Ferencz C, Rubin D, Mccarter RJ, Brenner JI, NeillC A, Perry LW, et al. congenital heart disease: Prevalence at Livebirth. The Baltimore-Washington Infant Study. Am J Epidemiol 1985;121(1):31–36.
6. Shah GS, Singh MK, Pandey TR, Kalakheti BK, Bhandari GP. Incidence of congenital heart disease in tertiary care hospital. KathmanduUniversityMedicalJournal2008; Vol6(1):33-36
7. Christianson AL. Down syndrome in sub–Saharan Africa. J Med Genet 1996; 33 (2): 89-92.
8. Khalil A, Aggarwal R, Thirupuram S, Arora R. Incidence of congenital heart disease among hospital live births in India. IndianPediatr1994; 31: 519-24.
9. Hassan I, Haleem AA, Bhutta ZA. Profile and risk factors for congenital heart disease. JPak MedAssoc.1997;47(3):78–81.
10. Fyler DC, Buckley LP, Hellenbrand WE, Cohn HE. Report on the New England regional infant care program. Pediatrics 1980;65(Suppl):375–461.
11. Burki MK, Babar GS. Prevalence and pattern of congenital heart disease. JAyub Med Coll Abbottabad 2001;13(4):16–18.
12. Khalil A, Aggarwal R, Thirupuram S, Arora R. Incidence of congenital heart disease among hospital live births in India.IndianPediatr1994;31(5):519–527.
13. Pattern of Heart Disease among neonates and their outcome: one year experience in non-invasive Cardiac Laboratory of Combined Military Hospital Dhaka. Major Nurun Nahar Tema Begum, Col Quazi Saifuddin Ahmed. Bangladesh Armed Forces Medical Journal 2002; vol xxix: 51-55.
14. Pattern of Congenital heart disease and treatment options in a Bangladeshi center: analysis of 6914 cases from noninvasive cardiac laboratory. Cardiovascular Journal 2017;9(2):97-105.